EVERYTHING YOU NEED TO KNOW ABOUT ACUTE
APPENDICITIS
Acute Appendicitis – Condensed Summary
1. Etiology
Luminal obstruction is the most common cause (≥50%)
Fecalith (appendicolith)
Lymphoid hyperplasia (especially in children and young adults)
Rare: tumor, parasite, foreign body
Obstruction → continued mucus secretion → ↑ intraluminal pressure → impaired venous return → ischemia + bacterial overgrowth → risk of perforation
2. Pathophysiology
Obstruction + inflammation → wall edema → lumen dilatation (>6 mm)
Advanced stage: necrosis, perforation, periappendiceal abscess
Location alters clinical and imaging findings (retrocecal cases may have more subtle findings)
3. Clinical Findings
Classic: Periumbilical pain → shifts to the right lower quadrant within hours
Fever, nausea, anorexia
Localized tenderness (McBurney’s point)
Rebound tenderness + guarding (peritoneal irritation)
However, atypical locations may not present with classic clinical findings
---
4. Locations of the Appendix
(Radiologically important as they alter both symptoms and signs)
Retrocecal: Most common (up to 65%), difficult to visualize with US, CT is more useful
Pelvic: Adjacent to bladder; may present with dysuria or pelvic pain
Subcecal: Beneath the cecum, easy US window
Paracecal: Medial or anterior to the cecum
Preileal / Postileal: Rare; may mimic right upper quadrant pain
Promontory: Near the pelvic promontory, atypical location

Retrocecal

Paracecal
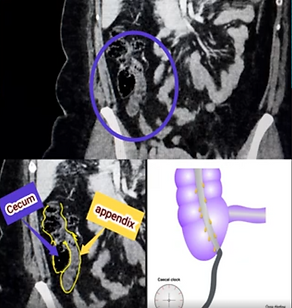
Subcecal

Promontory

Pelvic
💡💡💡💡If you want to see the detailed, annotated axial and coronal CT images of the cases shown in the pictures, watch the video.
5. US Findings (First-line, especially in young patients and pregnancy)
Blind-ended, non-compressible tubular structure >6 mm in diameter
Wall thickening (>2 mm)
Hyperechogenicity of periappendiceal fat (inflammation)
Appendicolith hyperechoic with posterior acoustic shadowing
Increased mural vascularity (Doppler)
Abscess appears as a heterogeneous mass
6. CT Findings (Gold standard, especially in atypical cases and obese patients)
Blind-ended, dilated appendix (>6 mm)
Wall thickening and contrast enhancement
Increased density (fat stranding) in periappendiceal fat planes
Appendicolith hyperdense (80–140 HU)
Complications: abscess, free air (perforation), phlegmon

CT findings of Appendicitis
7. Special Pearls
Location changes both clinical and imaging findings → CT is essential if US is negative in atypical positions
Lymphoid hyperplasia is the most common cause in children and young adults
In pregnancy, the appendix location shifts upward with gestational age → diagnosis becomes more difficult
Presence of an appendicolith increases the risk of perforation
On CT, wall thickening and degree of fat stranding help in staging
8. Complications
1. Perforation
Definition: Disruption of the integrity of the appendiceal wall, with intraluminal contents and bacteria spreading into the peritoneal cavity.
US Findings:
Focal defect in the appendiceal wall
Irregularity of wall contour
Periappendiceal collection or free fluid
In advanced cases, the appendiceal lumen may not be visualized (collapse or fragmentation)
CT Findings:
Periappendiceal free air (most
specific finding)
Low-density fluid + marked inflammation in fat planes
Findings of localized or diffuse peritonitis
Focal loss of the appendiceal wall or loss of contrast enhancement
2. Periappendiceal Abscess
Definition: Localized purulent
collection formation following perforation.
US Findings:
Heterogeneous, complex, fluid-containing mass
Reverberation/dirty shadow if gas is present
Marked surrounding hyperemia
CT Findings:
Thick-walled fluid collection with peripheral contrast enhancement
Air bubbles inside (evidence of perforation)
Marked fat stranding in surrounding adipose tissue
3. Phlegmon (Inflammatory Mass)
Definition: Inflammatory conglomeration of the appendix, surrounding fat, bowel loops, and omentum.
US Findings:
Mass appearance with marked echogenicity increase
Appendiceal lumen may not be visualized
CT Findings:
Soft tissue density mass around the cecum
Marked inflammation of fat planes
May contain minimal fluid, no well-defined capsule
---
4. Diffuse Peritonitis
Definition: Widespread intra-abdominal infection caused by perforation.
US Findings:
Diffuse free fluid
Decreased peristalsis of bowel loops
CT Findings:
Diffuse free fluid + free air
Diffuse bowel wall thickening
Diffuse peritoneal contrast enhancement
5. Pylephlebitis (Septic Thrombosis of the Portal Vein) – Rare but lethal
Definition: Portal vein infection and thrombosis secondary to
appendiceal origin.
US Findings:
Hyperechoic/anechoic thrombus in the portal vein
Loss of flow on Doppler
CT Findings:
Filling defect within the portal vein (thrombus)
Septic embolic foci in the surrounding liver parenchyma
Presence of an accompanying abdominal infection source
💡 Pearl:
CT is superior in diagnosing complications of perforation, but in a hemodynamically unstable patient, US is critical for rapid screening.
If US is negative, CT must be performed, especially if the location is atypical or if complication is
suspected.